Medication nonadherence is a pervasive challenge with far-reaching consequences for individual patient outcomes, population health, and healthcare costs. Yet, within this complexity lies a significant opportunity for healthcare marketers to lead the charge in redefining how we address adherence. By creating a seamless, patient-centered experience that integrates messaging across various points of care (POC) and offers consistent reminders, alerts, and support, marketers can be the architects of a more cohesive system that truly supports patient health.
Traditionally, the burden of addressing nonadherence has been placed squarely on patients or their physicians, often overlooking the fragmented nature of patient journeys, the sporadic nature of care, and the limitations of relying on patient self-reporting. This conventional approach is no longer sufficient in a healthcare landscape that demands more integrated and proactive solutions.
Healthcare marketers have the unique ability to develop a comprehensive approach to medication adherence by tracking patient interactions across multiple touchpoints and embedding themselves into the daily lives of patients. This strategy should prioritize enhancing patient understanding, eliminating adherence barriers, simplifying medication routines, educating and integrating care teams, and ensuring a seamless transition between in-person and digital touchpoints. However, to drive meaningful change, marketers must first challenge their existing assumptions about the barriers to adherence and take a holistic view of the nonadherence landscape.
Jump to Your Area of Interest
Intentional vs. Unintentional Nonadherence
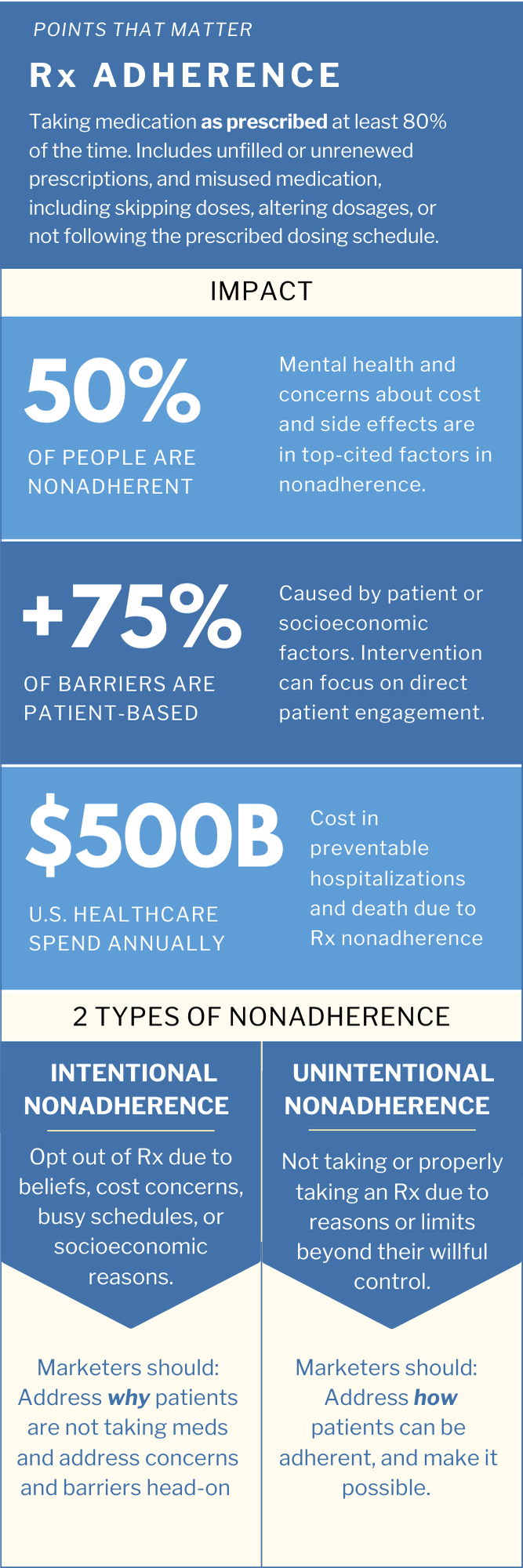
Adherence is more nuanced than many might assume. According to the American Medical Association, medication adherence is defined as taking medication “as prescribed” 80% of the time (AMA 2023). It is not just about whether patients pick up and take medication, but that they follow prescribed usage instructions 80% of the time for the medication to be effective.
Failure to adhere to these instructions can render the prescription ineffective, leading to significant immediate and downstream effects on patient outcomes and potentially altering broader perceptions of the drug.
Nonadherence manifests in two forms: intentional and unintentional, each requiring distinct intervention strategies.
Intentional nonadherence occurs for a variety of reasons, such as medication beliefs, cost concerns, or a lack of perceived necessity, leading patients to abandon prescriptions, skip doses, or alter their medication regimen.
Unintentional nonadherence arises from factors like forgetfulness, cognitive challenges, or physical difficulties in managing medication.
Both types of nonadherence are often exacerbated by underlying issues like shame or depression, which can prevent patients from honestly reporting their adherence struggles to healthcare providers.
It’s important to note that the term “noncompliance” may be misleading, as it implies that patients are willfully neglecting their treatment. In reality, the reasons for not taking medications as prescribed are often complex, multifaceted, and vary in degree, reflecting challenges that go beyond mere refusal or negligence.
Barriers to Medication Nonadherence
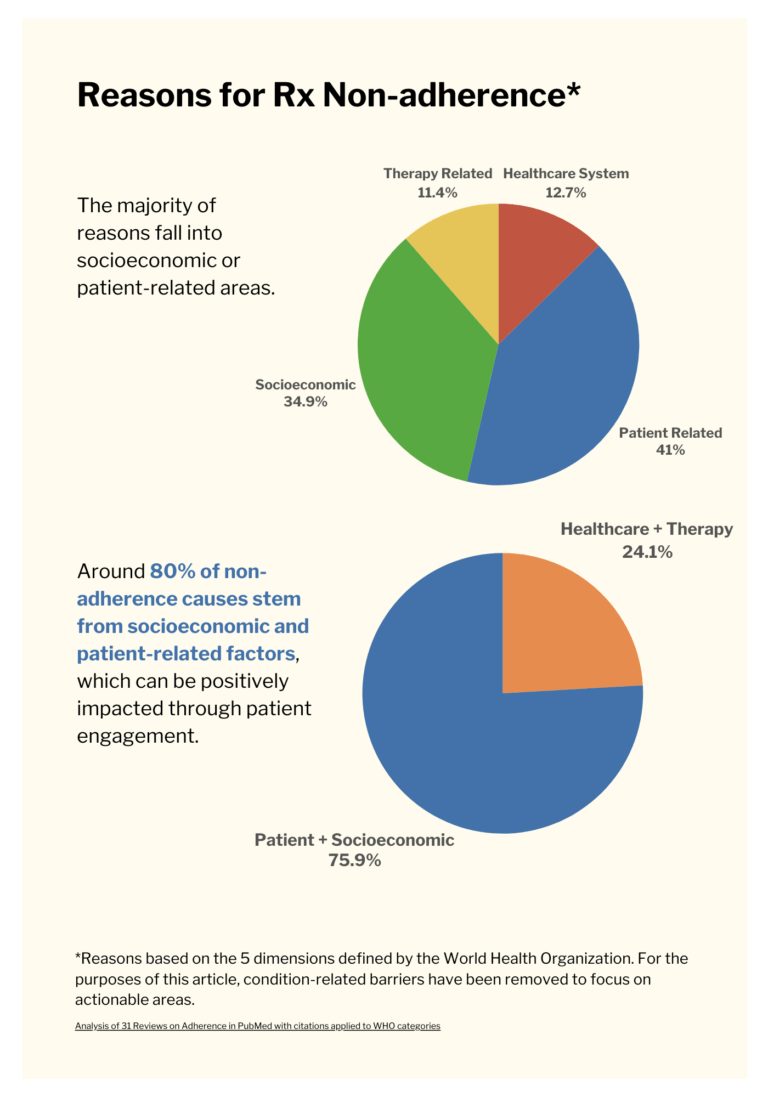
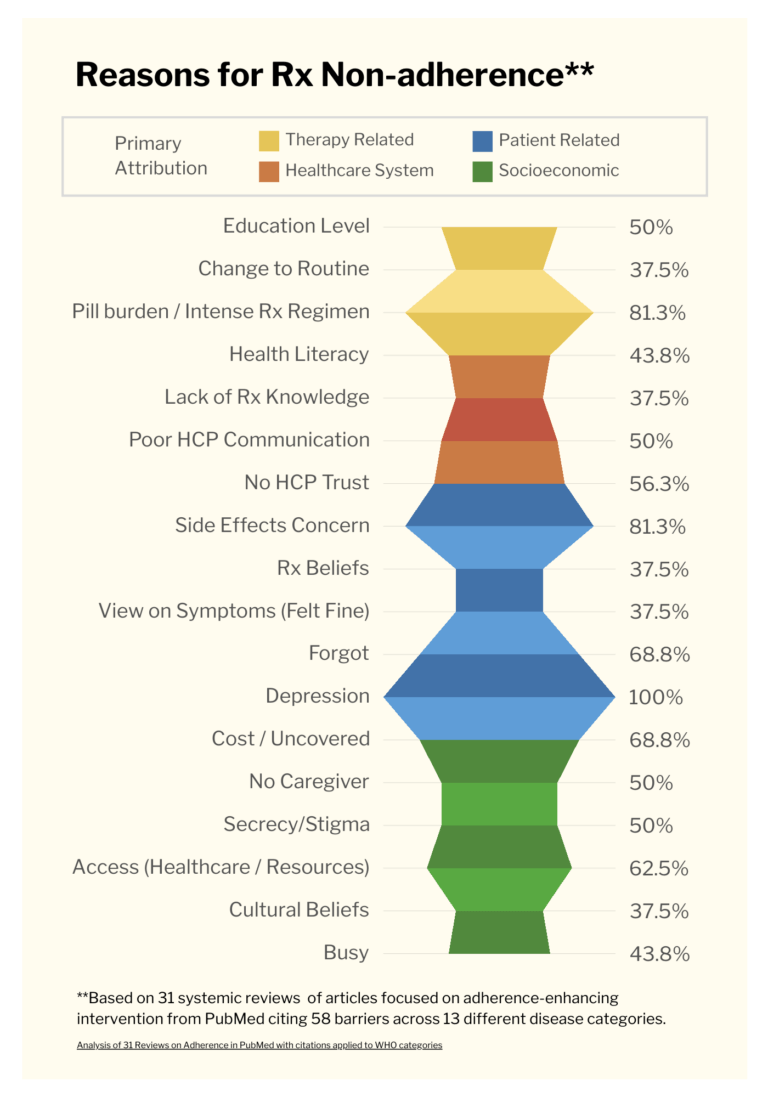
For point of care marketers, understanding these barriers is key to targeting and tailoring resources for patients and practitioners at specific care points. Drilling down into specific barriers and where they exist can identify the problems and solutions POC marketing can address. The top-cited barriers to adherence marketers can impact (see figure below), largely fall under two umbrella categories when abstracting strategically from the World Health Organization’s dimensions of adherence. (Source meta analysis: Divine et al 2018)
- Healthcare system centered barriers include therapy-related and healthcare system dimensions where it was on the non-patient side to provide effective information and communication about conditions and medications or to offer additional patient support.
- Patient centered barriers encompassing patient-related and socioeconomic dimensions, may also result from inadequate information, but are influenced by a person’s individual and sociocultural context, such as accessibility issues, psychological state, level of education, medication beliefs, or a history of noninclusive patient experiences.

Removing Rx Barriers at the Root
Drive Adherence: Focus on Patient-Centered Solutions and Education
Adherence intervention strategies should target the root cause of the barrier, with the vast majority (nearly 76% of barriers) being patient-centered and addressable by engaging directly with the patient. Evaluating a systematic review of barriers to adherence (2018), referenced in the following tables, we can see that the opportunity for direct intervention is ample. While complementary HCP-focused approaches are valuable, there is a strategic distinction between the primary responsibilities of healthcare providers and the independent resources that can complement or enhance healthcare efforts:
Target Real Touchpoints: Engage People Where It Matters Most
Patient education is critical to helping increase adherence, which is incredibly important in understanding the right marketing and engagement touchpoints. When examining the barriers to adherence, it’s clear that many barriers can be effectively addressed by providing patients and caregivers with direct information, resources, and support. This helps them better understand, access, and take their medications as prescribed. For example, barriers like beliefs about medications or cultural factors that affect trust in healthcare providers often require direct patient engagement and awareness campaigns. These efforts can be strengthened by leveraging points of care and community locations outside of traditional clinical settings.
Among the nearly 76% of adherence barriers that originate in the patient population, may could be addressed head-on at the Point of Care or other direct touchpoints. Below are the incidence rates doctors reported seeing barriers:
Patient Education as a Nonadherence Intervention
Looking at the above table, it’s evident that Patient Education alone could address the staggering rate of nonadherence relating to the amount of easy-to-understand information patients have and how it addresses concerns.
POC patient education could raise adherence in the following areas:
- 43.8% of patients struggled with health literacy
- 37.5% of patients lacked Rx knowledge
- 50% of patients experienced insufficient HCP communications
- 81% of patients had concerns about side effects impacting adherence
- 37.5% had cultural beliefs that impacted adherence
Adherence Solutions: When to Focus on Patients vs. Healthcare Systems
The bulk of the above medication adherence barriers can be addressed by POC engagement that delivers highly relevant information on medications, patient support, and resources at the right point in the patient journey. (See tables below.)
Patient-related behaviors and socioeconomic barriers can be addressed by patient-facing communications, while healthcare system and therapy-related barriers, often resulting from health-literacy or communication issues and poor visibility into patient data, present opportunities for point of care tools and HCP-assistance.
PATIENT CENTERED ADHERENCE SOLUTIONS
HEALTHCARE SYSTEM CENTERED SOLUTIONS
TARGET AUDIENCE: Patients and social systems (caregivers, family, community, etc) are the target audiences and the source of adherence barriers.
CHALLENGES MARKETERS CAN ADDRESS:
- Lack of understanding or information about conditions and medication
- Patient beliefs or concerns about medication or treatment unaddressed
- Noninclusive of patient identity or unrelatable
- Culturally or personally untrusted sources or approaches
- Low health literacy
- Mental and emotional states not considered
- Unable to afford or access prescribed treatments or medications
- Inadequate patient support
- Inconvenient or difficult treatments or medication routines
TARGET AUDIENCE: Healthcare systems and HCPs are target audiences, and source and location of adherence barriers.
CHALLENGES MARKETERS CAN ADDRESS:
- Inadequate communication around conditions and medication
- Ineffective communication strategies
- Not attentive or attuned to patient beliefs
- Lack of understanding of patient / overall health journey
- Multiple care providers / fragmented information
- Reliance on patient reporting / self-advocacy
Affordability Both Drives and is Driven by Adherence
Once diagnosed, the same patients who eagerly searched for solutions to medical conditions often don’t pick up or fail to take medications as directed. “Some 50% of Americans don’t take their medications as directed by their doctor, for any of a host of reasons. This non-adherence leads to preventable hospitalizations and preventable deaths, and costs 16% or $500 billion of the entire U.S. healthcare spend every year.” (PSQH 2022)
Cost concerns play a dominant role in nonadherence and abandonment across demographics and access levels. According to IQVIA (2020), when a medication is seen as expensive (over $500), unfilled prescriptions jump from 5% to 60%. Cost concerns drive patients to prioritize other expenses, change or skip dosages, or develop negative beliefs about medications, leading them to seek alternatives. Such behavior not only affects patient outcomes and public health but also has a significant impact on healthcare, prescribers, and pharmaceutical companies (IQVIA 2020).
Nonadherence has far-reaching consequences beyond what patients realize. Undertreated or untreated conditions can lead to increased lifetime healthcare costs, secondary problems, and extended diagnostic work (AMA 2023).
Ironically, affordability concerns that drive nonadherence may ultimately contribute to higher drug prices. As Drug Discovery Today (2023) states, “High medication adherence is not only important to achieve the expected treatment effects but can also effectively reduce medical costs.”
Point of Care Tactics Can Address Cost Concerns
Specific POC strategies and tactics can address patient cost concerns, removing the largest barrier to care. For example, healthcare marketers can:
- Leverage the EHR and bring-in HCPs: Enable prescribers through Electronic Health Records to identify drug options and couponing opportunities at the time of prescribing (PSQH 2022)
- Empower patients with information: Provide pricing transparency and realistically affordable medication and pharmacy options
- Be Upfront About Nonadherence: Offer materials on the dangers of medication misuse at the time of prescription or in-bag at pickup.
- Dedicate Resources to Affordability Assistance: Create support lines, guidance, and other dedicated patient-support to address financial and insurance related concerns, questions, and navigation
Find the right point of care marketing solution with the Point of Care Marketing Product Finder tool. Tailor solutions specifically to your healthcare marketing needs based on the following selection criteria: point of care setting, target audience, specialty / specialty location, media tactic, and product lines.
Physician Rx Blindness and Adherence
Doctors are not frontline in battling nonadherence, yet treatment evaluation and decisions rely heavily on patient adherence. There are many reasons patients may not report problems interfering with intentional or unintentional adherence.
Patients may mistakenly believe their providers are aware of nonadherence.
Patients may be reluctant to talk to doctors about how or whether they are taking medications.
Patient conditions, emotional state, or accessibility may limit ability to correctly self-report
Patients go to multiple doctors
Patient medications or health routines are confusing
Patients go too infrequently to prescribing doctor
Lack of trust or trusted relationship with prescriber
Lack of caregiver or advocate to help with communication
For POC marketers, helping providers understand and address concerns, identify patients with barriers, and equipping them with inclusive communication strategies and tools can help address noncommunication.
Additionally, helping patients report more accurately or automating medication tracking for easier reporting may triage this noncommunication. Medication trackers, wearable interactive alerts, pharmacy apps, and print or digital medication journals could be integrated into patient-doctor experiences or portals. Many can also help log side effects and symptoms that may impact patient adherence.
Of course, with any technology, resolving adherence issues means making it simple for patients to use, sustain, and share information. Automating wherever possible helps.

Why the Language around Adherence Matters
It’s important that we get the language right to keep our mindset as marketers focused on creating patient-centered messaging. There is a key distinction between adherence and compliance. (Tasaduq 2023) Adherence shows a willingness to take medication, relying on patient disposition, aptitude, and behavior. Importantly, “Adherence, when defined appropriately, means that the patient has a choice to receive or not to receive needed treatment” (Adherence Versus Compliance 2023). The takeaway is:
- With intentionally nonadherent patients, we need to answer why they are not adherent and give them reasons to take medications that address concerns or barrier beliefs head-on.
- White unintentionally nonadherent patients, we need to answer how they can be adherent, and make it possible.
This nuanced definition is mission-critical because when we talk about adherence, these are all areas that POC marketers can help with. POC marketers can create information and content that boosts confidence, understanding, and action. We can develop patient-centered messaging that addresses the specific and varied factors influencing adherence, improving medication adherence and, ultimately, patient outcomes.
Pharmacists Can Help Unintentional and Intentional Nonadherence
Pharmacists are well positioned to identify behaviors that spur medication nonadherence. (Read more on Pharmacy’s role in patient intervention in our blog.) As a high-impact point of care, pharmacists can:
- Leverage patient relationships to encourage patient sharing
- Engage with caregivers and/or have visibility into familial and care status
- Handle questions about medications and side effects
- Introduce or work with tools, like punch cards or pharmacy apps, to help patients remember and routinize medication and the correct way to take them
- Problem solve issues around adverse effects or physical limitations, including offering dietary or over-the-counter aids to help maintain medication routine (upset stomach, dehydration, digestion, bowel functioning, etc)
- Help patients with cost savings and navigation.
Which pharmacy a patient goes to can play a role in adherence, especially around intentional nonadherence related to costs or busy schedules. Not all patients know about pharmacy options and how strongly it can impact cost, or would know how to competitively shop. POC materials and tools can help patients find the best cost-to-access pharmacy option to boost medication taking.
Strategic POC/Healthcare Marketing Tactics and Considerations
Intuitively leveraging point of care marketing makes sense, but the machinations of marketing often mean investment in these critical engagement strategies is lost to disparate initiatives or oversight. Integrating point of care is a strategic master play that, done effectively, lightens patient and HCP burdens, removes adherence barriers, and heightens marketing ROI. One case study (Crossix) showed an ROI of 8.5x the investment in a 100M campaign resulting in POC driving 17% of the NBRx attribution when paired with digital and television. By leveraging point of care marketing and tools, healthcare marketers can transform medication adherence and drive patient satisfaction.Some considerations include:
-
Develop educational materials that increase understanding and support for patients and caregivers
-
Provide medication reminders, alerts, and dosage tools to help patients stay on track
-
Support and integrate care providers to increase transparency, create safe spaces for questions, and equip patients and caregivers with the information they need
-
Embrace healthcare consumer behavior by leveraging digital portals, apps, and trending POC locations to create a seamless messaging experience across touchpoints
-
Tailor POC strategies to specific barriers of care, targeting healthcare system-facing and patient-directed solutions
By understanding and addressing the barriers to medication adherence, POC marketers can create meaningful interventions that improve patient outcomes and drive positive change in the healthcare industry.